A recent report offers health care guidance for physicians, nurses, pharmacists and other professionals treating those with a history of elevated exposure to PFAS.
The National Academies of Sciences, Engineering and Medicine released the report last week. It also suggests ways the Center for Disease Control and Prevention can update its health recommendations for patients with PFAS exposure.
Supporter Spotlight
Perfluoroalkyl and polyfluoroalkyl substances, or PFAS, are a class of chemicals with more than 12,000 different compounds found in thousands of products, such as carpeting, nonstick cookware, firefighting foams, fast-food wrappers and protective gear.
Used since the 1940s for its oil- and water-repellent properties, PFAS have a variety of distinct chemical properties and toxicities, some of which can become concentrated in the body or environment and stay there, while other PFAS can transform pretty quickly, the report states. “The PFAS that do transform, however, will become one or more other PFAS because the carbon–fluorine bond they contain does not break naturally,” which is why they’re described as “forever chemicals.”
The report found that there’s “sufficient evidence of an association” between PFAS exposure and a greater risk of decreased response to some vaccines, abnormally high cholesterol, decreased infant and fetal growth, and increased risk of kidney cancer. Additionally, there is suggestive evidence of an association for increased risk of breast cancer, liver enzyme alterations, increased risk of pregnancy-induced hypertension, increased risk of testicular cancer, thyroid disease and dysfunction, and increased risk of ulcerative colitis.
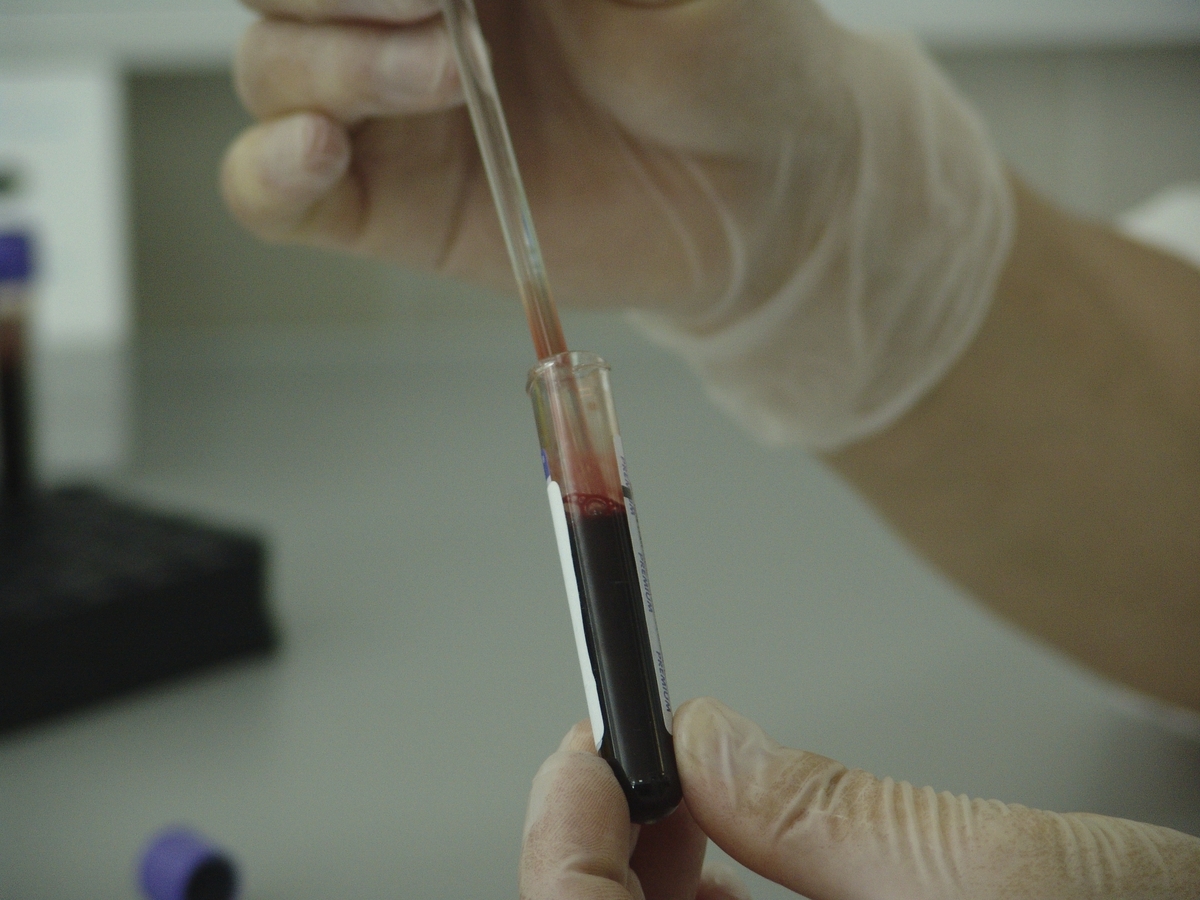
As a result of these connections between PFAS exposure and health risks, the report recommends that clinicians should offer PFAS testing to patients that are likely have a history of elevated exposure. The report also recommends that those patients with PFAS levels linked with an increased risk of adverse effects should receive regular screening and monitoring by their health care professionals. The report notes that establishing these recommendations came with challenges because there’s a great deal of uncertainty, such as what level of exposure comes with what type of health risks.

Dr. Jane Hoppin, a professor of biological sciences and the deputy director of the Center for Human Health and the Environment at North Carolina State University, is on the committee the National Academies of Sciences, Engineering, and Medicine appointed to develop the report.
Supporter Spotlight
“I think this report actually provides guidance for people who have been exposed to PFAS. The recommendation is that people with more than 2 nanograms per millimeter total PFAS in their blood should receive some kind of medical follow-up and those people with more than 20 should receive more,“ Hoppin told Coastal Review Friday.
She said that about 9% of people exceed that 20 nanograms per milliliter value, and some parts of the United States probably have higher exposure.
“PFAS exposure is widespread throughout the U.S. and particular regions of the United States have higher exposures. What this report really does is, for the first time, provides medical recommendations for people who’ve been exposed to PFAS,” she said.
When blood was monitored in the past, researchers have only been able to say the number of nanograms in a person’s blood. “But now, what this report does, not only does it say that if this is your number, this is what should be done, but also gives guidance for clinicians on how they should do that. So I think that’s a really important point here for North Carolina and the U.S. as a whole.”
Recommendations
Hoppin was referring to the levels of PFAS concentration found in patients.
Patients whose tests show a PFAS blood concentration below 2 nanograms per milliliter are not expected to have adverse health effects, according to the report. Patients with test results between 2 and 20 nanograms per milliliter could face the potential for adverse effects, especially in sensitive populations such as pregnant individuals. Patients with test results above 20 nanograms per millimeter may face a higher risk of adverse effects.
Patients who test between 2 and 20 nanograms per milliliter should prioritize screening for dyslipidemia, hypertensive disorders of pregnancy, and breast cancer based on age and other risk factors.
Clinicians with patients who have more than 20 nanograms per milliliter should also test thyroid function and assess for signs of kidney cancer, testicular cancer and ulcerative colitis during all visits.
In addition to regular monitoring of patients, the study recommends that clinicians discuss with their patients ways to avoid PFAS exposure. There also should be improvements in environmental health education, particularly in communities where PFAS exposure is identified.
Clinicians should also discuss infant feeding and steps that can be taken to lower sources of PFAS exposure, though the report notes that there is a critical need for more data to understand exposure among breastfed infants.
To get the word out to clinicians and the public, the report states that the CDC, Agency for Toxic Substances and Disease Registry, and public health departments should create educational materials on PFAS exposure, possible health effects, what can be learned from and the limits of testing, and the benefits and negatives of testing.
Laboratories conducting PFAS testing should report the results to state public health authorities to improve exposure surveillance.
Study background
The Agency for Toxic Substances and Disease Registry released in 2019 “PFAS: An Overview of the Science and Guidance for Clinicians on Per- and Polyfluoroalkyl Substances.”
While this overview provided general information about PFAS health studies and suggested answers for example questions from patients, the guidance did not provide information for clinicians on when to test for PFAS, how to order the tests, how to interpret the results or follow up, according to the report.
In response to the frustration voiced by some in PFAS-impacted communities that the clinical guidance lacked clear recommendations, the registry and National Institute of Environmental Health Sciences approached the National Academies of Sciences, Engineering and Medicine to form an ad hoc committee to give advice on PFAS testing and clinical care for patients exposed to PFAS.
The committee was asked to advise on principles for biological testing and clinical evaluation, given substantial scientific uncertainty about the health effects or the value of such measures in informing care; review the human health literature for the health effects of PFAS; and characterize human exposure pathways and develop principles for exposure reduction, the report states.
The committee also was asked to recommend options and considerations to guide decision making for PFAS testing in a patient’s blood or urine, PFAS concentrations that could inform clinical care of exposed patients, and appropriate patient follow-up and care specific to PFAS-associated health endpoints for those patients known or suspected to be exposed to PFAS.
The committee was not asked for community prevention guidance or advice on policies that would reduce PFAS exposure, the report notes.
Uncertainty
There are 2,854 locations in the country, all 50 states and two territories, that have some PFAS contamination, but not all exceed the level in health advisories, and almost 100% of the country’s population is exposed to at least one PFAS.
The report acknowledges that though there is uncertainty about the exact nature of risks from PFAS exposure, clinicians will still need to advise and make decisions with patients regarding their exposure.
“While there is evidence of an association of PFAS with several health outcomes, the likelihood that a particular individual will have any specific adverse health outcome following exposure to PFAS cannot currently be determined with great specificity,” the report states. Adding, that while there are gaps in information about how individuals can reduce any potential risks related to PFAS exposure, many individuals and communities expect clinicians to address PFAS-associated risks as part of routine health care delivery.
“Ongoing and future research should eventually guide clinicians in predicting patient risk and provide an understanding of the benefits and harms of interventions designed to avoid adverse health outcomes,” the report continues.
“Our report shows that we are going to need robust and effective collaboration between local communities, states, and federal agencies in order to respond to the challenge of PFAS exposure,” said Ned Calonge, associate professor of family medicine at the University of Colorado, Denver, associate professor of epidemiology at the Colorado School of Public Health, and chair of the committee that wrote the report. “We need to continue to identify communities with elevated PFAS exposure, learn more about specific health impacts, make testing available to patients, and give clinicians more strategies for counseling patients and providing preventive medical care.”
PFAS in North Carolina
Residents of Bladen, Brunswick, New Hanover and Pender counties learned five years ago that their primary source of drinking water, the Cape Fear River, was contaminated with GenX and other emerging PFAS. The Wilmington StarNews first reported on June 7, 2017, that a group of North Carolina State University researchers had detected the forever chemicals in the river.
The following week, the state’s Department of Environmental Quality and Department of Health and Human Services began investigating. The Chemours facility in Fayetteville was identified as the company producing the GenX that was being discharged into the Cape Fear. Since then, the state and environmental groups have worked to clean up the Cape Fear River.
A consent order was signed in February 2019 between NCDEQ, Cape Fear River Watch, represented by the Southern Environmental Law Center, and Chemours. The order requires Chemours to address PFAS sources and contamination at the facility to prevent further impacts to air, soil, groundwater and surface waters. In August 2020, NCDEQ made an addendum to the consent order, making Chemours take significant additional actions to prevent PFAS pollution from entering the Cape Fear River. A summary of actions over the last five years related to the Chemours investigation and consent order is on the NCDEQ website.
A representative from DHHS told Coastal Review that the state agency is still reviewing the report but work is underway to incorporate information from this report and other sources in an update of the state’s guidance to North Carolina health care providers.
Expanded PFAS testing in blood and serum could potentially help identify areas that have increased exposures to PFAS chemicals, and provide residents with more information to help understand their exposures and how they could be impacting their health, DHHS officials said.
Community voices
The committee brought in public input, which they deemed “an important and credible source of evidence to inform guidance recommendations.”
As part of that effort, 41 community liaisons, including a handful from North Carolina, were appointed to suggest speakers, topic and discussion questions for public meetings, as well as provided documents and other information.
Dr. Jamie DeWitt, an associate professor in the Department of Pharmacology and Toxicology of the Brody School of Medicine at East Carolina University, was selected as a community liaison. She focuses on the effects of environmental contaminants on the adult and developing immune systems and is the principal investigator, co-principal investigator, and co-investigator of several funded studies on the immune effects of PFAS, particularly the novel and understudied.

“The report does something that has been needed for a long time with respect to people who live in any community that can be contaminated with environmental chemicals,” DeWitt said Monday. “It really alerts healthcare providers that there are agents in the environment that can have an impact on people’s health, and they can look for tools to help them treat their patients better, and help to uncover potential health risks that their patients might experience as a result of their exposures.”
DeWitt mentioned that she teaches medical students and while students across the country learn about acute toxicology such as poisoning or snake bites, they don’t really learn about how environmental agents can lead to chronic diseases. DeWitt noted that the report addresses medical education and highlights ways that healthcare providers can better educate themselves to provide care for people who live in communities that are contaminated with PFAS.
The committee held several public comment sessions as well as included in the report the testimony of 30 people impacted by PFAS contamination, which “moved the committee’s work from an academic exercise to a personal reality.”
Clean water advocate Beth Markesino, founder of North Carolina Stop GenX in Our Water, is a community liaison who shared her story with the committee during a public comment session.
A Wilmington resident, Markesino, who participated in the first GenX study, has multiple endocrine issues associated with PFAS, including a thyroid tumor, an adrenal tumor, and placenta problems during her pregnancy that resulted in the death of her son.
Her organization was awarded a grant to provide 120 filters for low-income residents in the Lower Cape Fear region and she lobbied against DuPont scientist Michael Dourson’s appointment to the Environmental Protection Agency.
“I started North Carolina Stop GenX In Our Water the day that we found out about our water contamination, so on June 7, 2017,” she said. “We started the organization as a way to inform our community about our water contamination.”
The group first began on Facebook, but after learning the urgency of the situation, the group became a nonprofit organization.
“The National Academies of Sciences, Engineering and Medicine had reached out to a bunch of not only North Carolina advocates, but also advocates throughout the United States wanting to know our opinions about PFAS and health and data,” she said. “Out of every other state, I want to say we got a very good representation of our water contamination and our views, which was really great. In the last five years, it might seem like we haven’t got a lot accomplished, but we really have and with this report coming out, this catapults us to a whole new level.”
She and her husband moved to the Wilmington area for the weather. As a marathon runner, she said she was drinking a lot of water. She became pregnant with her son in 2016, when she was in the best health of her life.
“We had no clue about our water contamination in 2016. You know, none of us knew the health effects of PFAS or anything like that. And long story short. My pregnancy did not go very well. I already had a very healthy pregnancy with my daughter and my daughter’s 10. Now she’s an amazing sassy, little 10-year-old, but with my son Samuel, he did not develop his kidneys, bladder or bowels and I had placental problems,” she said.
They found out around 20 weeks through the 24-week period that she had next to no amniotic fluid … “Just think about your worst nightmare. And that was it for me.”
She ended up in Michigan to deliver their son at 24 weeks via cesarean because a natural birth would have caused health complications. “We did get to hold Samuel. We got to baptize him, and we got to bury him in our family plot in Detroit.”
Six months after they buried their son and were grieving, “that’s when we found out about a Gen X contamination,” Markesino said. “As a pregnant mom, I never knew our water was contaminated. I never knew that drinking this water could possibly affect my pregnancy. Five years later, we know that PFAS and Gen X does affect pregnant women, it does transfer from the placenta to the fetus.”
Being a community liaison for the study made her feel like she could help other women that are pregnant be able to talk to their doctors about PFAS.
“We may not have known it five years ago, when I was going through all of that, but we know it now and through committees like this that I was a part of — many of us in the PFAS community have similar stories to mine and my son who have shared our stories and shared our concerns with this committee and even though we couldn’t fix the pain and agony — we shared our stories so that doctors can be educated and that they can now tell their patients about the science now that we know of the harm of these chemicals, so that nobody else has to go through what we went through.”